F.A.Q
FAQ
General
There have been a few patient records which Dr. Champion has already
received from her previous locations. However, we
are asking the majority of patients to complete a release form so our office
may professionally request your records.
(Click
here for Records Release Form.)
Patients may also access their own records via the prior office’s portal system. This has proven to be a more direct and efficient way. Reach out to Dr. Champion’s staff if you need assistance with this method.
Receiving prior records is beneficial for your appointment but it is NOT a requirement. We want to address your eye care needs, regardless of record status.
Champion Eye Care accepts assignment with Medicare and secondary plans. We also participate with many major insurance providers, including:
- All Blue Cross Blue Shield PPO and HMO
- All Cigna PPO and HMO
- Aetna
- Medicare Part B
- Tricare for Life
- Tricare Select PPO
- United Health Care
- Wellmed Medicare HMO
Our office is working tirelessly to become in-network with all carriers. If you have questions about a particular insurance not listed here, please contact us.
It is solely Dr. Champion at this time, but we hope to keep growing and add further staff to optimize all your eye care needs! Please check back for any updates.
FAQ
Eye Conditions
Many people living with dry eye feel misunderstood and unsatisfied with their treatment, according to a new survey. Health Union interviewed 415 Americans with chronic dry eye about their experience managing the condition. Here’s what the survey found, and what ophthalmologists say could help.
The most frustrating thing about dry eye is ...
Difficulty finding relief from dry eye symptoms
Frustration with how dry eye is diagnosed or perceived
Struggling with the debilitating symptoms of dry eye
Experts say dry eye is often mistaken for other conditions
Dry eye is one type of ocular surface disease, a group of disorders that causes the eyes to not produce enough tears or the right quality of tears. Tears are essential for keeping your eyes healthy and comfortable. “Ocular surface disease is very complex with many subtypes and overlapping symptoms. Getting to a correct diagnosis requires expertise and can take time,” says dry eye expert Christopher Starr, MD, an associate professor of ophthalmology at Weill Cornell Medical Center. “A lot of symptoms are labeled and treated as dry eye, but patients may not be getting better because there are other things going on” he says. Allergic conjunctivitis, blepharitis, meibomian gland dysfunction, floppy eyelid syndrome, corneal dystrophies and toxicity to medications or cosmetics are just a handful of the many conditions that can be incorrectly referred to as dry eye disease, Starr says. While artificial tears can provide temporary relief in many of these cases, they don’t treat the underlying causes.
Here are the best tools and tests for diagnosing dry eye
“People who are feeling frustrated should not give up. There are a growing number of diagnostic tools to pinpoint the root problems and an expanding number of treatments to address them,” Starr says. Eye doctors may also use other tests that measure the quality of tears. They may also perform imaging tests to look for problems with the meibomian glands, which produce an oil found in healthy tears.
Treating dry eye is tricky, but not impossible
There are many treatment options today and finding a solution may involve some trial and error. Many people find it necessary to combine therapies and make a few lifestyle changes. The right treatment regimen can involve a lot of daily maintenance.
Your eye doctor may suggest:
Age-related macular degeneration (AMD) is a problem with your retina. It happens when a part of the retina called the macula is damaged. In this article: With AMD you lose your central vision. You cannot see fine details, whether you are looking at something close or far. But your peripheral (side) vision will still be normal. For instance, imagine you are looking at a clock with hands. With AMD, you might see the clock’s numbers but not the hands. AMD is very common. It is a leading cause of vision loss in people 50 years or older.
Two types of AMD
Dry AMD
This form is quite common. About 80% (8 out of 10) of people who have AMD have the dry form. Dry AMD is when parts of the macula get thinner with age and tiny clumps of protein called drusen grow. You slowly lose central vision. There is no way to treat dry AMD yet.
Wet AMD
This form is less common but much more serious. Wet AMD is when new, abnormal blood vessels grow under the retina. These vessels may leak blood or other fluids, causing scarring of the macula. You lose vision faster with wet AMD than with dry AMD. Many people don’t realize they have AMD until their vision is very blurry. This is why it is important to have regular visits to an ophthalmologist. He or she can look for early signs of AMD before you have any vision problems.
Who Is at Risk for AMD?
You are more likely to develop AMD if you:
Having heart disease is another risk factor for AMD, as is having high cholesterol levels.
Age-Related Macular Degeneration Diagnosis
During an eye exam, your ophthalmologist may ask you to look at an Amsler grid. This grid helps you notice any blurry, distorted, or blank spots in your field of vision. Your ophthalmologist will also look inside your eye through a special lens. He or she can see if there are changes in the retina and macula. Your ophthalmologist will put dilating eye drops in your eye to widen your pupil. This allows him or her to look through a special lens at the inside of your eye. Optical coherence tomography (OCT) is another way to look closely at the retina. A machine scans the retina and provides very detailed images of the retina and macula. Optical coherence tomography angiography (OCTA) is another way to look closely at the blood vessels in and under the retina. This is like fluorescein angiography but does not use a dye.
Age-Related Macular Degeneration Treatment
Dry AMD treatment
Right now, there is no way to treat the dry form of AMD. However certain people with lots of drusen or serious vision loss might benefit from taking a certain combination of nutritional supplements. A large study (AREDS and the later AREDS 2 study) found those people may slow their dry AMD by taking these vitamins and minerals daily:
Your ophthalmologist can tell you if vitamins and minerals are recommended for your dry AMD, as not all forms will benefit from the AREDS supplements. Beta carotene should not be used by smokers as it raises the risk of lung cancer.
Eye-healthy foods
Dark leafy greens, yellow fruits and vegetables, fish, and a balanced, nutrient-rich diet have been shown beneficial for people with AMD.
Wet AMD treatment
To help treat wet AMD, there are medications called anti-VEGF drugs. Anti-VEGF treatment helps reduce the number of abnormal blood vessels in your retina. It also slows any leaking from blood vessels. This medicine is delivered to your eye through a very slender needle.
Making the Most of the Vision You Have
If you have AMD, you can learn how to make the most of your vision. Often you can still do many of your favorite things with special low vision tools. These can include different kinds of magnifying tools, handheld computers, electronic items and more. Also, you can learn how to use your side vision to help you do things. A vision rehabilitation specialist can teach you how this works. They also can help you find many low vision support services and tools. Ask your ophthalmologist to help you find a vision rehabilitation specialist in your area. The goal is to learn new ways to be as independent as possible.
Test Your Vision with the Amsler Grid
AMD causes your vision to change over time. You may not notice these changes when they happen. But you need to catch vision changes as soon as possible. Treating them early can help slow or stop further loss of sight. You should use an Amsler grid every day to monitor your vision. One is below for you to use.
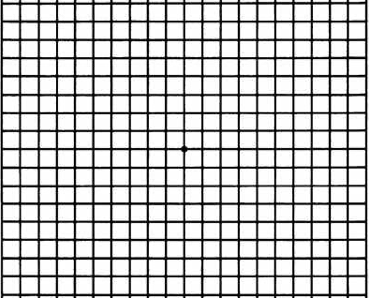
Here is how to use the Amsler grid:
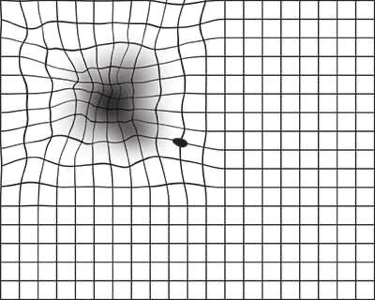
This is what an Amsler grid might look like with blurry, wavy lines, or dim areas.
FAQ
Cataracts
Cataract surgery costs are generally covered by Medicare if you are Medicare eligible. Private insurance usually covers cataract surgery as well.
Medicare will cover your costs if your vision tests at a certain level of acuity or clarity. Private insurance plans may have similar vision requirements. If your surgery is covered you may still have some costs. Special types of IOLs will cost more. Choosing to have cataract surgery before your vision has deteriorated enough will cost more.
In certain cases, it might be possible to get coverage before you meet the age or vision requirements. Talk with your ophthalmologist if you are considering having early cataract surgery.
What do you do if you don't have Medicare or private insurance coverage? You may still be able to reduce and manage the cost of cataract surgery. Ask about payment plans through your doctor's office. See if your employer offers flexible spending accounts that can help. Your ophthalmologist can help you learn more about costs of cataract surgery. Discuss your options for affording the procedure.
Aging is the most common cause. This is due to normal eye changes that begin to happen after age 40. That is when normal proteins in the lens start to break down. This is what causes the lens to get cloudy. People over age 60 usually start to have some clouding of their lenses. However, vision problems may not happen until years later.
Other reasons you may get cataracts include:
Most age-related cataracts develop gradually. Other cataracts can develop more quickly, such as those in younger people or those in people with diabetes. Doctors cannot predict how quickly a person’s cataract will develop.
Posterior capsulotomy is laser surgery you might need sometime after cataract surgery. It helps you see clearly if your vision becomes cloudy again. When you have cataract surgery, your ophthalmologist removes your eye's cloudy lens. They replace it with a clear, artificial intraocular lens (IOL). The IOL is held in place in the eye’s natural lens capsule. Weeks, months or years later, this capsule can become cloudy or wrinkled, causing blurry vision. This is called a posterior capsule opacification (PCO). It’s also sometimes called a "secondary cataract" or "scar tissue." With posterior capsulotomy, a laser is used to make an opening in the cloudy capsule. This allows light to pass through again for clear vision.
What Happens During Posterior Capsulotomy?
The procedure is done in your ophthalmologist's office. It only takes about 5 minutes. Here is what will happen:
What Are the Risks of Posterior Capsulotomy?
As with any surgery, there are possible risks and complications with posterior capsulotomy. Here are some of them:
FAQ
Types of Glaucoma
Primary open-angle glaucoma
This is the most common type of glaucoma. It happens gradually, where the eye does not drain fluid as well as it should (like a clogged drain). As a result, eye pressure builds and starts to damage the optic nerve. This type of glaucoma is painless and causes no vision changes at first. Some people can have optic nerves that are sensitive to normal eye pressure. This means their risk of getting glaucoma is higher than normal. Regular eye exams are important to find early signs of damage to their optic nerve.
Angle-closure glaucoma (also called “closed-angle glaucoma” or “narrow-angle glaucoma”)
This type happens when someone’s iris is very close to the drainage angle in their eye. The iris can end up blocking the drainage angle. You can think of it like a piece of paper sliding over a sink drain. When the drainage angle gets completely blocked, eye pressure rises very quickly. This is called an acute attack. It is a true eye emergency, and you should call your ophthalmologist right away or you might go blind. Here are the signs of an acute angle-closure glaucoma attack:
Many people with angle-closure glaucoma develop it slowly. This is called chronic angle-closure glaucoma. There are no symptoms at first, so they don’t know they have it until the damage is severe or they have an attack. Angle-closure glaucoma can cause blindness if not treated right away.
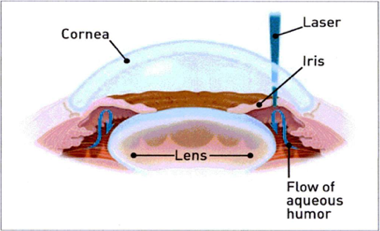
What is a YAG PI? (Laser Iridotomy)
Laser iridotomy is a procedure to create a small hole in the colored part of the eye, called the iris, with a laser. This procedure helps treat or prevent angle-closure glaucoma. Glaucoma is an eye disease in which the nerve that carries visual messages to the brain (optic nerve) is damaged. This is usually caused by high pressure inside the eye. Damage to the optic nerve can cause a permanent loss of vision. Glaucoma needs to be diagnosed and treated early to prevent blindness. Normally, the fluid in the front of the eye is constantly flowing from where it is formed (the ciliary body) to the front of the eye. This fluid nourishes your eye and helps to keep its shape. The area between the iris (colored part of the eye) and the cornea (the clear outer layer on the front of the eye) is called the angle. Fluid drains out through the angle, into drainage channels, and is then reabsorbed by the body. When fluid flows out too slowly, eye pressure builds up.In angle-closure glaucoma or attack, the angle between the iris and the cornea is blocked or narrowed. When this happens, fluid is not able to drain from the eye. This can cause a pressure buildup.
When is it used?
Laser iridotomy helps restore the proper flow of fluid in the eye and reduce eye pressure. In most cases, this laser operation can successfully control eye pressure and preserve your vision. Without the procedure, you could permanently lose your vision. If you have had an attack of angle-closure glaucoma, you may be in pain and may have nausea and vomiting in addition to sudden loss of vision. The iridotomy is done as an emergency procedure in these cases. This procedure is also done in some people who are at high risk for getting angle-closure glaucoma. You may be at high risk if:
How do I prepare for this procedure?
No special preparation is necessary. You may drive yourself to the appointment, and home after the procedure. Some patients prefer to bring a family member along, but this is not necessary.
What happens during the procedure?
Your eye provider will put drops in the eye to lower pressure and keep you from feeling pain. Your provider may also put a special contact lens on the surface of the eye. A very short laser pulse will then be pointed at the eye. You may feel a quick pinch in your eye and hear a snapping noise. It is important to try to keep your head and eye still during the procedure and avoid jumping back. If you have an angle-closure glaucoma attack, this is an emergency procedure.
What happens after the procedure?
The provider will remove the contact lens. Your eye will be rinsed out with some saline, and you will have you eye pressure checked about 15 to 20 minutes after the procedure. If this was an emergency procedure, it may take some time for your vision to return to its previous level and for the eye pressure to come back to a more normal level. In rare cases, another surgery is needed to control the eye pressure. You will need a follow-up appointment to check your eye pressure and the results of the procedure. You may need to have the same laser procedure in the other eye to prevent angle closure.
What are the risks of this procedure?
Your healthcare provider will explain the procedure and any risks. In general, the risks of laser iridotomy are small compared to its potential benefit. Some possible risks include:
Every procedure or treatment has risks. Ask your healthcare provider how these risks apply to you. Be sure to discuss any other questions or concerns that you may have.